Background Information
Insomnia is one of the most prevalent sleep disorders, affecting up to 20% of adults and placing a heavy burden on both individual well-being and public health systems. Pharmacological treatments—though widely used—carry risks like dependency, side effects, and diminished daytime functioning. Behavioral therapies like Cognitive Behavioral Therapy for Insomnia (CBTI) show strong results, but only a minority of patients achieve full remission. Amid this treatment gap, interest in meditation as a complementary therapy has grown.
Mindfulness meditation aims to reduce stress and promote present-moment awareness without judgment. Mindfulness-Based Stress Reduction (
MBSR
Mindfulness-Based Stress Reduction (MBSR) is a program designed to help individuals cope with stress, pain, and illness. Developed by Jon Kabat-Zinn in the 1970s, it combines meditation and yoga to promote awareness and stress management. The eight-week program teaches participants to focus on the present moment non-judgmentally, enhancing their ability to manage difficulties.
More on Wikipedia
View in glossary
), a popular structured program, has shown promise across a range of stress-related conditions, including insomnia. In this study, the authors introduce and evaluate a new program, Mindfulness-Based Therapy for Insomnia (MBTI), which integrates mindfulness techniques with behavioral strategies like sleep restriction and stimulus control.
What They Did
This
Randomized Controlled Trial
A Randomized Controlled Trial is a scientific study design that randomly assigns participants to either an experimental group receiving an intervention or a control group, allowing researchers to measure the true effect of the intervention while minimizing bias.
More on Wikipedia
View in glossary
enrolled 54 adults diagnosed with chronic insomnia and compared three groups: (1) a standard 8-week MBSR program, (2) an 8-week MBTI program that adds insomnia-specific behavioral techniques, and (3) a self-monitoring (SM) control group that tracked their sleep but received no treatment during the initial 8 weeks.
Participants reported their sleep in daily diaries and completed standard measures including the Insomnia Severity Index (ISI) and the Pre-Sleep Arousal Scale (PSAS). Objective sleep data were gathered using polysomnography and actigraphy. Follow-ups occurred immediately after the 8-week program and again at 3 and 6 months.
One Big Result
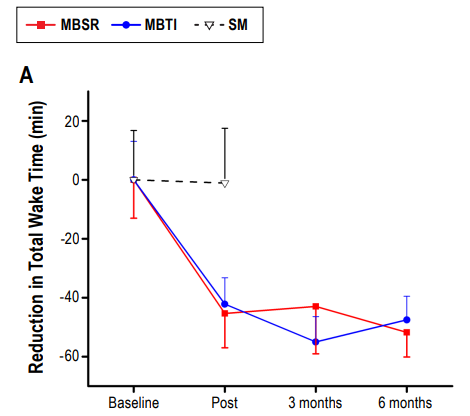
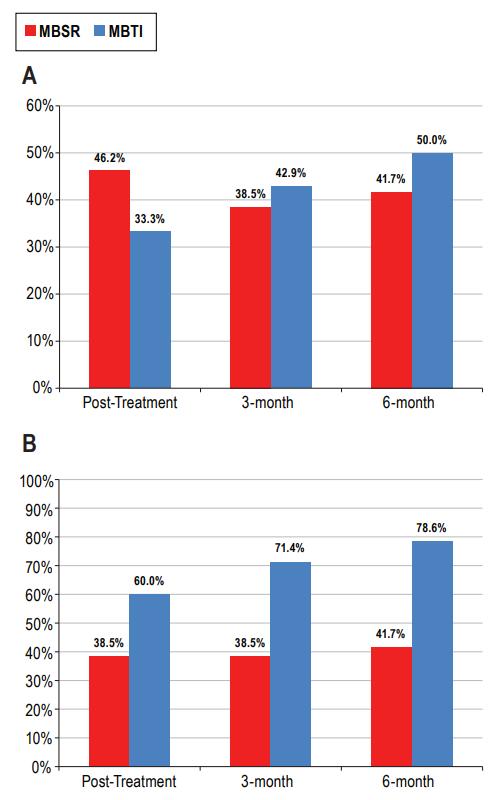
Both MBSR and MBTI participants showed a large reduction in total wake time—averaging 44 minutes less awake at night by the end of the treatment, compared to virtually no change in the control group. These improvements were sustained or improved over the following six months. MBTI participants, in particular, showed the greatest long-term reduction in insomnia severity, with 79% meeting criteria for treatment response and 50% achieving full remission at six months.
Participants who received either MBSR or MBTI reported a mean reduction in total wake time from baseline to post-treatment of 43.75 minutes and from baseline to the 6-month follow-up of 49.63 minutes.
Mindfulness meditation, especially when combined with behavioral strategies, significantly reduces nighttime wakefulness and the severity of insomnia.
Miscellaneous Interesting Takeaways
Meditation Reduces Sleep-Related Arousal
Participants in the meditation groups reported marked reductions in pre-sleep arousal (mental and physical tension before sleep), a key contributor to insomnia. These reductions were not observed in the self-monitoring group.
Psychological Engagement Matters
Participants in both MBSR and MBTI adhered to their home meditation practice, logging between 1,400 and 2,000 minutes of practice over the study. MBSR participants practiced slightly more, but MBTI participants had better long-term sleep outcomes, suggesting that the content of the practice—especially behavioral integration—matters.
Objective Measures Lag Behind
While participants subjectively reported major improvements, objective measures like polysomnography and actigraphy showed smaller and less consistent changes. This aligns with prior research indicating that mindfulness impacts how we experience sleep more than it alters raw sleep architecture.
Sixty percent of participants who completed MBTI had a minimally important treatment response at post-treatment, with the rates rising to 78.6% at the 6-month follow-up.
Meditation May Appeal to Specific Populations
The study sample was predominantly composed of highly educated women—demographic groups that are more likely to seek out and benefit from CAM therapies like mindfulness. This suggests meditation may be especially effective for individuals already inclined toward self-regulation and mind-body approaches.
Final Reflection
Mindfulness meditation offers a compelling non-pharmacological alternative for people with chronic insomnia, especially when paired with practical behavioral strategies. It helps people not just sleep longer, but worry less and rest better.
Citation
Ong, J. C., Manber, R., Segal, Z., Xia, Y., Shapiro, S., & Wyatt, J. K. (2014). A Randomized Controlled Trial of Mindfulness Meditation for Chronic Insomnia. Sleep, 37(9), 1553–1563. 10.5665/sleep.4010